COVID-19 is a disease which impacts various parts and systems of the human body.
“The digestive system is not immune from the effects of COVID-19,” said gastroenterologist Dr. Mohammed Al Haddad. “We notice that one out of three or four can have digestive symptoms, some of them have abdominal pain, nausea, diarrhea and some have acute liver issues.
“Some patients develop acute pancreatitis,” he added.
Haddad said that the nausea and diarrhea can both require hospitalization. Nausea can prevent people from keeping food or drinks down and diarrhea can impact hydration and electrolytes. He said the symptoms tend to subside once the virus has worked its way out of the digestive system.
He said that some patients tend to have diarrhea, nausea or cramps that take a few months to subside. And the long-term impact of COVID-19 on the digestive system is “something that’s (still) being studied.”
But for those with chronic pancreatitis, he’s noticing a trend.
Patients with chronic pancreatitis who then develop COVID-19 “tend to have relapses for up to a year and that’s something that hasn’t been researched,” said Haddad, the pancreas is among his specializations within gastroenterology.
“I plan to do a write-up on that, the impact of COVID-19 on the chronic pancreatitis,” he said.
Pandemic changes how gastroenterologists work
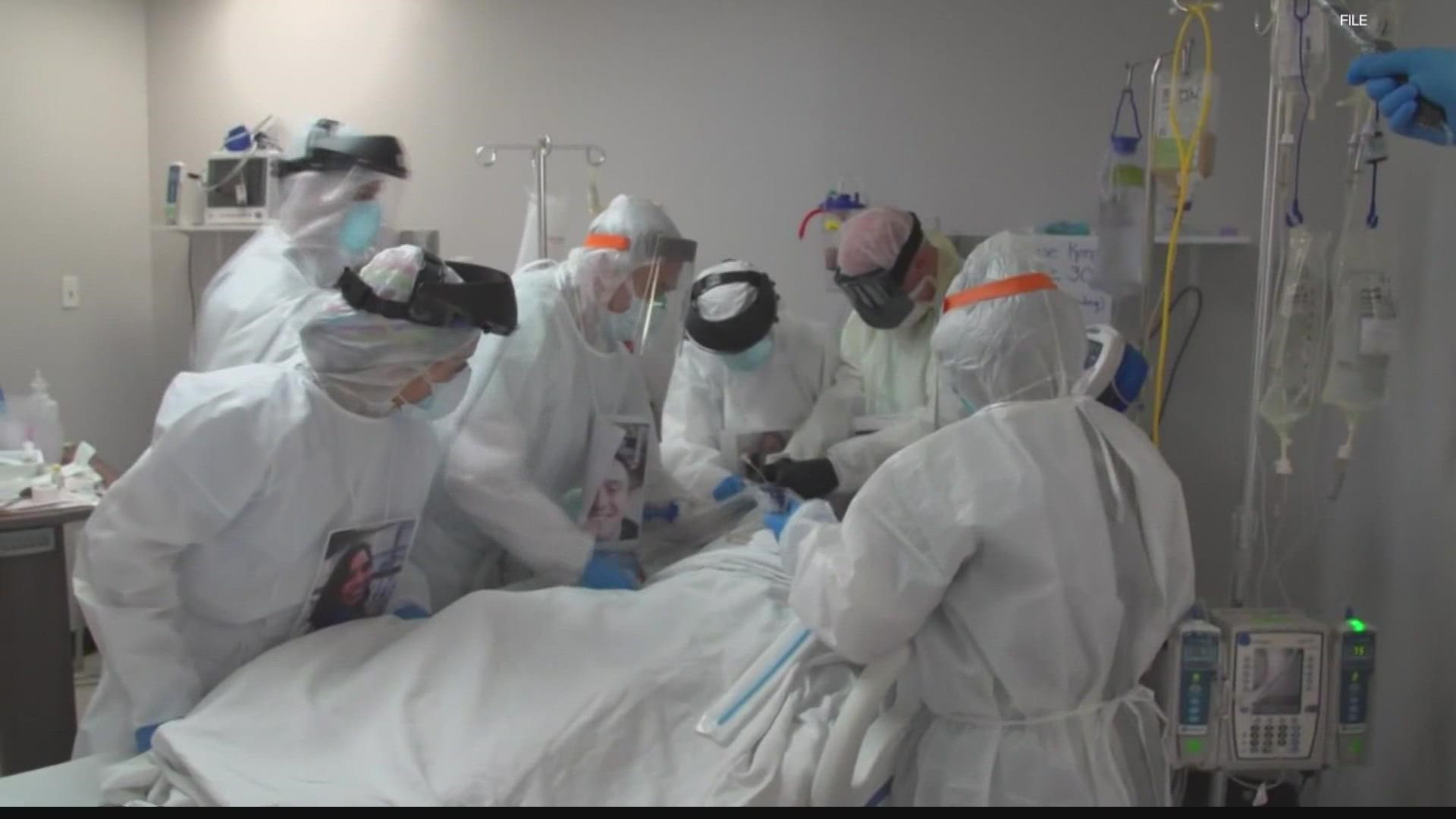
Endoscopies are pretty routine procedures, but the pandemic has changed the way they’re done. Patients are tested for COVID-19 ahead of all procedures and for confirmed COVID-19 patients, “we request full sedation instead of twilight sedation,” said Haddad.
He said that he and his staff are returning to “heavier PPE equipment,” but they’re “not too concerned like we were back in the spring of 2020.”
But the capacity to take care of patients is still a concern if staff have to call out sick or quarantine.
“Even if you get an illness that keeps you home for five days, that’s five days away from the hospital,” said Haddad.
It's not about ICU beds
Haddad remembers during the second surge when the vast majority of ICU beds, “around 80%” belonged to COVID-19 patients. He said that there are more ICU beds available right now during the current surge.
“Three or four beds out of ten beds in the ICU are being occupied by a COVID patient,” he said.
But most hospitals have also increased the number of ICU beds since the start of the pandemic.
“I can tell you our biggest problem isn’t beds or equipment,” Haddad said. “(It’s) staff(ing)."
He said that healthcare workers are going back to quarantining and getting tested and at any given time, some members of his staff are out as a matter of safety and precaution.
“We were able to expand beds, but we weren’t able to increase the number of healthcare workers,” Haddad said.
He said the healthcare industry had hoped to attract more people, but hasn’t been able to attract enough to keep up with the strain the pandemic is causing across the country.
“Our bandwidth isn’t just restricted by space, but personnel as well,” Haddad said.


The doctor said he doesn’t think this third wave is going away anytime in the immediate future
“I think it’s going to be another 7-8 weeks or 2-3 months 'til we see a decline,” Haddad said.
He said the majority of critically ill patients are unvaccinated.
“This is a disease that happens by choice rather than lack of choice,” the doctor said. “Of course we don’t discriminate, but it’s hard to keep that level of empathy among team members knowing that some patients had the choice of getting out of the ICU for over a month and they passed it on. And then they say, ‘I wish I had taken it because I’d be in much better shape."
Toll on healthcare workers
“The stress and anxiety among my doctors and nurses and respiratory therapists is at an all-time high,” said Haddad. “And they’re not getting a break.
“I can assure you if you work in the ER or ICU consistently you are extremely prone to PTSD.” He said the mental toll it’s taken on the frontline is one that “will require long term mental health support,” and is something that should be watched and attended to.
The pandemic has brought many dark days, especially during the spring of 2020.
“We didn’t have much protective equipment, we just didn’t know a lot about the virus, and we were seeing a lot of people dying,” said Haddad, referring to March and April of 2020.
“It was tough to swallow that,” he added. “Seeing people who were quite healthy and within days they were on the ventilator and died."
He said the vaccine helped to bring some brighter days.
Brighter days
“Those old and frail people who we knew would come to us (and be admitted), weren’t coming to us or if they were they were coming for a few days and then they’d leave,” said Haddad, reflecting on his patients after the vaccine. “It was remarkable!”
He said he was very excited when he himself could get the vaccine and that he posted a photo on social media to encourage others to get vaccinated as well.
Haddad said knowing that scientists "came together to serve humanity when everything was falling apart" is humbling and inspiring to the next generation of healthcare workers and scientists.